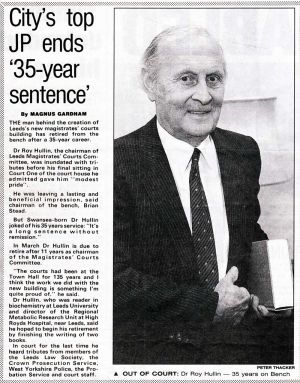
Dr Roy Hullin
I am privileged to have finally met the highly respected Dr Roy Hullin and his wife Freda, who have given generously of their time and mementos, to be included in this archive. Sincerest thanks to Freda, who with foresight started collecting this material in scrapbooks dating from 1953.
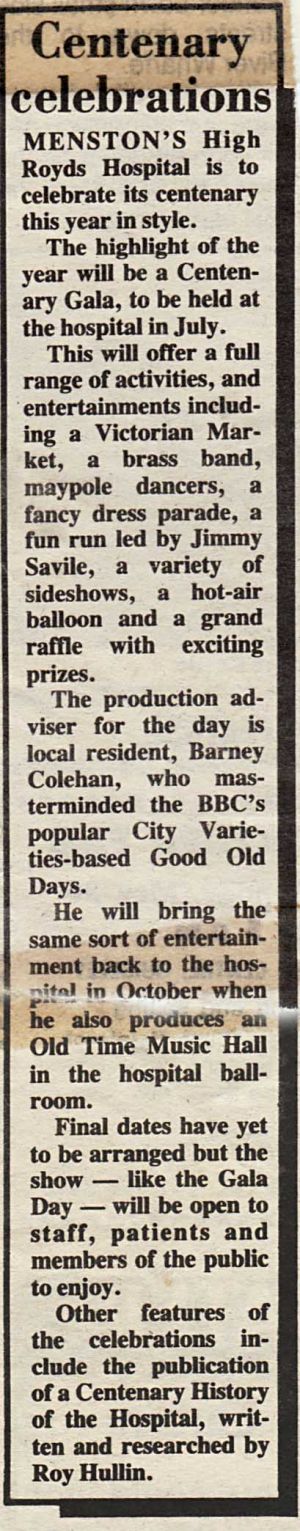
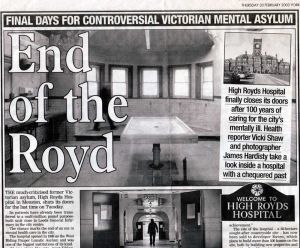
Undoubtedly, Dr Hullin’s work has indelibly advanced the field of Metabolic Research and his service to High Royds Hospital is recalled with genuine fondness by all those who came into contact with him in the course of his illustrious career. Dr Hullin also undertook the wonderful compilation of the history of the hospital for the Centenary Brochure 1888-1988. It is a remarkable piece, worthy of separate attention which has certainly helped in the creation of this archive. You can find the brochure in the front page index of collections.
…………………………………………………………………………………
November 1953
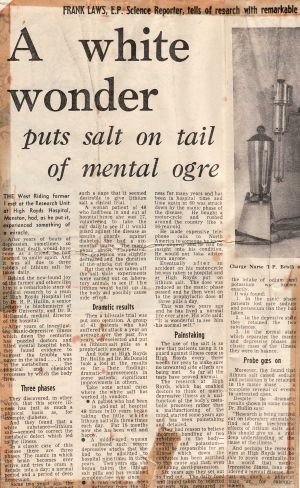
Important discovery in mental treatment
By a Yorkshire Post Reporter
Two Leeds University scientists have made a discovery which could result in a more specific method of treating a mental disorder: manic depressive psychosis.
The scientists Dr. J. Dawson and Dr. R.P. Hullin, members of the staff of Professor F.C. Happold, Head of the Biochemistry Department of the University- discovered that certain chemical changes in the blood are related to changes in the moods of patients suffering from the illness.,
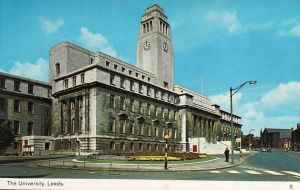
Yesterday when he formally opened the new laboratories of the Biochemistry Department of the University, in Hyde Terrace, Sir. Rudolph Peters, Whitley Professor of Biochemistry at Oxford University described the discovery as a “chemical clue which may well lead to new knowledge of some important detail of the brain tissue,” and said it was easy to see why the management committee of the mental hospital at Menston and the Medical Research Council supported the research work.
At Menston Hospital, blood and other changes of a number of substances are being determined over the three to four months cycle of illness of a few individual patients. Collected information is being correlated with mood changes.
Dr.Dawson told me yesterday that he and Dr.Hullin had discovered that certain products of sugar break down changed with a change in the mental state, and they were interested in finding out what determined these changes in the chemical substances and how far present methods of treatment were successful in affecting these chemical substances. Present methods of treatment were efficient but empirical; their discovery could result in a more specific method of treatment by drugs.
Opening the laboratories, Sir Rudolph Peters said biochemistry was virtually as active , perhaps even more so, than atomic physics. They must have the space to train more biochemists so that they could meet the demands of those who wanted them. All professors of biochemistry must have the humiliating experience of not being able to find men for good posts. They must also have space for the research and for the training in research, and, in addition, they must have apparatus.
Sir Hubert Houldsworth, Pro Chancellor of the University described the new laboratories ( adapted from what was previously a nursing home, at a cost of £15,000) as another development of the university.
Thanking Sir Rudolph for opening the laboratories, Professor Happold said they were doing fundamental research and applied research in university departments and they were training men and women for life in applied science. Without generous assistance from the University Grants Committee and industry the work would not be possible.
Sir Charles Morris, the Vice Chancellor, was among the large number who attended the opening ceremony.
…………………………………………………………………………….
Metabolic Research
Rather than being seen as the poor relation to other hospitals in and around Leeds, Menston began to attract research in its own right, with the University of Leeds Department of Biochemistry starting work on its first project there as early as 1952. In 1962 a Metabolic Research Institute was set up, and subsequently published dozens of scientific papers in leading journals, giving the hospital an international reputation in the field of biochemical research into mental disorders.
One treatment pioneered at Menston was the use of lithium to prevent recurrent episodes of depression and mania. Lithium was first developed in 1949, and had dramatic results, holding out hope for a cure and release for thousands from the shadows of the asylum.
In later years other work at Menston would expand to look at senile dementia and the role of nutrition.
…………………………………………………………………………………..
A Talk With Dr Roy Hullin
I am extremely grateful to have been given the opportunity to speak with Dr Roy Hullin and his wife Freda. They made me feel most welcome and it was a privilege to record some recollections from Roy’s esteemed medical career which I can share with you.
Roy
I graduated in Swansea in 1944 and at that time you were told where you would be employed. Those at the top of the exam list were usually given an option of looking at approved posts and not necessarily going to the forces. I had a degree in physics and chemistry at that time and often such candidates went in to radar. As chance came, I went to an approved job as Research Chemist in Boots Drug Co. Nottingham. I enjoyed the work on anti tuberculosis drugs and my desire developed to help people in a general way. By 1947 after three years at Boots, they relaxed the Essential Works Order, so you could look around at other posts. You previously were expected to stay at the job and had to do a 40 hour week. Boots had inherited a 5 day week, or it was brought in by Jesse Boot, so we had to boost the hours to 40 by working longer days but you did have weekends free. I could have stayed at Boots they were happy to have me but decided to look around.
At the end of my time there I saw a post advertised at Cardiff City Mental Hospital, Whitchurch, which had an interesting history and had been doing biochemical studies since 1915. It was unusual for a hospital to have a lab in those days. The post was advertised by the Medical Research Council – by now I had met Freda and we were engaged to be married in the September so I wanted to be nearer to her as she lived in Neath. I was interviewed in London, got the job and came back to Neath. Freda had just been discharged from the WRNS.
I had not previously known anything about mental illness and when I started the job the Director of Research, Derek Richter, tasked me with the study of the brains of mental patients, obviously after death. There was of course no control over supply, so I spent most of the first two years or so, collecting the brains of psychiatric patients. As a comparison I had to get normal brains from the main hospital in Cardiff, so I would rush around to collect available brains and bring them back to Whitchurch and process the brains get out cell nuclei from cerebral cortex and place them in the large centrifuge at Whitchurch.
We found one interesting thing, some of the determinations showed a significant difference and that was from brains of patients suffering from senile dementia. Only a very few people around the world were researching this area.
I became very interested in mental disorder and stayed there three years and completed my PHD. Then in 1949 the Universities had been given money through the ICI Research Fellowships. I applied with my project looking at mental disorder. I got the Fellowship and began now the research on live patients with a professor Happold the Governor of the Quaker, York Retreat. I spent three years studying patients there. One aspect that fascinated me was that many patients seemed to have a fluctuating illness, swinging from periods of depression, periods of normality and episodes of mania. A pattern emerged so I pursued this through the Retreat and started looking at electrolytes and there were indeed significant changes through these fluctuations.
Most of us control our sodium levels within very fine limits. It is finely balanced and large doses would naturally come out of the body in 24 hours. I found that patients in periods of depression retained sodium and would not excrete it, then when they improved, it would come out. I became interested in studying the far swinging manic depressives so could study the fluctuations over a shorter period of time. Such research at the Retreat got me involved in Sheffield with another colleague so we followed these patients through cycles. 24 hr cycles, 72 hr cycles. Some patients were referred to me from Alec Jenner in Sheffield. One case, a boxer I recall with mania and depression was manageable when down but very difficult when up. His family learnt to cope and live around his fluctuations, planning events around periods of his depressions.
After my time at the Retreat I naively thought what I needed was to be able to repeat this study on a large number of patients. High Royds attracted me with over 2700 patients, it was overcrowded at the time. Wanting to then look at these patients, I would get masses of them brought to me. Some patients had been there 60 or 70 years. I started work there and I began to see the need for full metabolic studies. I needed to look at the fluctuating patients under homogenised feeding, and regular urine and faeces testing. This was very expensive from a nursing point of view. Fortunately, I had got to know the Councillor Mrs Hammond from The Fabian Society who was on the Hospital Committee at High Royds. The Medical Superintendent at the time, Charlie Gore had the power of control over the whole staff; doctors, nurses, the works, complete responsibility. One advantage, if I could convince the Mrs Hammond and Superintendent Gore I would be given everything I needed. I said I would need a small number of patients and 26 staff, you wouldn’t get that today. Within six weeks of my request I was given a laboratory, an empty doctors house for patients and the staff to carry out the research. Collecting all the specimens and doing balanced studies was not easy. The Metabolic Research Unit went on to be established in Escroft Clinic on site.
I was appointed Laboratory Director as well. The studies were very interesting and we achieved Medical Research Council support, so went on from there. Results led me to the use of Lithium in the fluctuating patients. This would dampen down the swings of illness. We collected data from all over the country to discover if patients were any better on lithium and they were. It changed many lives. I recall one grateful former patient, a manic depressive who had been Chief Gardener in The Parks Department and had lost his job through illness. He was an excellent gardener who had trained at Chatsworth House. He and his family were so happy with his improvement on lithium that he would turn up at early hours just to do our garden when we lived in Yeadon by way of thanks.
It was important to obtain good statistical evidence that lithium was successful so by the late 70s, after all the data and studies, the trial of 92 patients with the fluctuating condition, 82 of them were successfully treated with lithium which were positive results. It became a standard treatment. I then went on to carry out further studies on Alzheimers Disease.
…………………………………………………………………………………………………………..
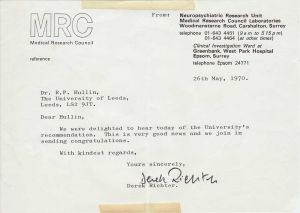
Derek Richter 1907-1995. Director Of Research Whitchurch Mental Hospital, Cardiff
Derek Richter, one of the founding fathers of modern neurochemistry, died on December 15, 1995 at the age of 88. He had a full and active life, the most important aspect of which for him was to strive, through research, to reach a better understanding of the working of the brain and to gain new knowledge that might help in the treatment of the mentally ill.
In 1947 he accepted a job as Director of Research in Whitchurch Hospital, Cardiff. The research history of Whitchurch was excellent, owing to the outstanding work previously carried out by Juda Quastel. However these research activities came to an end by the outbreak of war, and Derek had to build up everything from scratch in an environment that often interfered with, rather than promoted his efforts. Even in 1957 at the hospital, one had to get to the main laboratory through the pharmacy, negotiating a narrow passage under the scornful gaze of the hospital pharmacist, who made it clear that she thought the researchers were up to no good!. In spite of bad accommodation, obsolete equipment, and an unsympathetic medical superintendent, Richter developed exciting research. He succeeded in obtaining financial support frm the Medical Research Council and the Rockerfeller Foundation and recruited an excellent crew, amongst whom was Dr Roy Hullin. The team embarked upon pioneering neurochemical work.
………………………………………………………………………………………………………………………………..
Juda Hirsch Quastel, CC, FRS , FRSE (1899-1987) was a British-Canadian biochemist who pioneered diverse research in neurochemistry, soil metabolism, cellular metabolism, and cancer.
Quastel, also known as “Harry” or “Q,†was born and educated in Sheffield, Yorkshire, England. He served with the British Army as a Laboratory Assistant at St. George’s Hospital from 1917 to 1919.
Electing to study chemistry, Quastel received a baccalaureate from Imperial College London in 1921. Pursuing graduate work at Cambridge University, Quastel studied with Frederick Gowland Hopkins, the leading figure in British biochemistry and a future Nobel Prize recipient for his work on the nutritional importance of vitamins. Under Hopkins, Quastel received a doctorate of philosophy from Cambridge in biochemistry in 1924 and, not long after, was made a Fellow of Trinity College.
Quastel remained in Hopkins’ department as a demonstrator and lecturer from 1923 to 1929, during which he pioneered the research of microbial enzymology. He obtained a doctorate of science from Cambridge in 1926 and received a Beit Memorial Fellowship in 1928.
Quastel accepted a position as Director of Research at the Cardiff City Mental Hospital in 1930. From this location, he was able to conduct early work on the enzymology and metabolism of the brain. For these studies, Quastel was made a Fellow of the Royal Society of London in 1940.
……………………………………………………………………………………………………………………………………………………
THE BIOCHEMISTRY OF THE AFFECTIVE DISORDER
Dr R P Hullin
Director Of The Metabolic Research Unit 1952-1994
The possibility that biochemical changes may play a part in the production of mental disorders such as manic depressive psychosis has aroused much interest in recent years. The Metabolic Research Unit at High Royds has made its own contribution to this field, There are two obvious ways of assessing the biochemical factors associated with a mental disease, One is to study a large group of patients suffering from the disease and determine whether the factor is different from that in a similar group of mentally normal subjects.
The other method involves making serial observations on carefully-selected individual patients throughout the changing pattern of the affective disoder, The classical case of manic-depressive psychosis mannifests itself in alternating phases of mania and depression separated by mentally-normal periods. For research purposes the more frequent the cycles the more suitable is the patient for investigation. In the simplest form, the variables under study are determined regularly through successive mood cycles in order to discriminate between changes occurring randomly and those invariably associated with one particular time in the cycle. Any such change is not necessarily related to the affective state in a direct way Biochemical changes may be the result of many factors, e.g., the amount or composition of food or fluid intake or the physical activity of drugs.
The most reliable data are obtained when serial determinations are made in a patient who receives a constant, daily diet (i,e. containing approx. the same amount of protein, fat, carbohydrate, electrolytes, water etc.) and no drugs other than those whose effect is being studied. Obviously there are considerabie difficulties in carrying out such studies but broadly, we have managed to overcome most of them in investigations carried out in the Metabolic Research Unit, High Royds Hospital, since 1962. Three areas of research in the biochemistry of affective disorders which have excited great interest are (i) water and electrolyte distribution, (ii) corticosteroid secretion and metabolism, (iii) the relationship between brain monoamines and mood. The work at High Royds has mainly been concentrated on the first of these without completely neglecting the other two.
The experimental techniques used have included both the classical balance technique and the determination of body fluid compartments by the dilution principle. The principles underlying the balance technique are simple and well-known namely the determination of the dietary intake of a constituent and the relationship of this to its total excretion by the available routes. The institution of a suitable routine, with cross checks, the training of the nursing staff in its application, choice of co-operative patients – these are some of the difficulties common to all metabolic balance work, with mental patients, the development of good relationships is especially important in securing and maintaining the necessary minima1 level of co-operation. Some anticipated snags have not in fact occurred, probably due to the excellence ef the nursing staff available in the Unit.
Some of the results obtained in manic-depressive patients are:
(a) The extracellular fluid volume is maximal during normal phases decreasing in both the depressed and manic phase of the disorder.
(b) Recovery from depression, whether it occurs spontaneously without physical treatment or when accelerated by means of electro-convulsive therapy and/or anti-
depressive drugs is invariably accompanied by increases in the extracellular space and in total body water
(c) During changes from mania to depression, body water changes were in the opposite direction to these described above.
(d) Body weight changes reflect the underlying water changes, Some patients on a constant diet while still mentally normal lose up to 3Kg, in 3-4 days prior to the onset of depression. Conversely a marked gain in body weight unassociated with dietary change occurs during recovery from depression.
Studies in normal subjects by previous workers had suggested that alterations in emotional state might give rise to changes in the rate of excretion of water and sodium by the kidneys that cannot be accounted for by changes in intake. It is well known of course, that emotional stimuli provoke or inhibit diuresis in human subjects.
The metabolic balance studies have also revealed that the depressed phase in many patients is associated with a net gain of electrolytes, especially sodium. Manic phases, in contrast are usually periods of net sodium loss.
Although changes in electrolyte or water distribution are more likely to be the effect rather than the cause of affective illness, it is possible by making certain assumptions and applylng them to the central nervous system to postulate that they should lead to considerable changesin brain excitability. Although at first sight’ changes in brain excitability would be expected to have general effects on brain function not merely on mood, It is not impossible that the changes, might actually cause the depression or mania. The use of lithium salts which will effectively control, symptoms of mania and may also have a prophylactic effect in preventing recurrent epispdes of depression and mania is certainly of much interest in this respect and much of our work since 1964 has been concerned with the clinical effectiveness and metabolic effects of lithium salts.
Our studies have confirmed that lithium salts are therapeutically affective against 80% of manic phases, the effect differing qualitatively from that produced by neuroleptic drugs such as chlorpromazine or haloperidol. Although the latter act more rapidly than lithium, they produce at best an effective suppression of the manic overactivity and restlessness and bring the patients into what is in most cases, a drug-produced state of quietude; below the surface the elevated mood, flight of ideas and other symptoms of mania usually persist. Lithium by contrast, seems to remove the manic symptoms in a more specific manner; hyperactivity, restlessness, talkativeness sleeplessness etc.disappear without any sedation or production of lethargy and usually the patients do not feel drugged. However, long-term balance studies have shown that the administration of Lithium has far-reaching effects on electrolyte metabolism. Normal subjects given lithium generally reach an equilibrium position after 6 days in which the excretion of the lithium balances the daily dose, Manic patients on the other hand, usually retain some of the daily lithium so that a cumulative intracellular retention off the cation occurs. There is evidence that this retention of lithium may persist in some patients for periods of 6-12 months, When the treatment, is then-stopped, the retained lithium is slowly released into the plasma and urine in discrete episodes lasting 2-5 days separated by several weeks when lithium is not.
………………………………………………………………………………………..
Widely Reported In The Press:
£70,000 to Investigate a New Therapy. Report 1970
A grant of more than £70,000 made to Dr.R.P.Hullin, Senior Lecturer in Biochemistry will enable Biochemists at Leeds University to step up a programme of research into drugs which may alleviate a common mental disorder. A daily dose of lithium salts – substances known for over a hundred years â appears to reduce the symptoms of mania and the Medical Research Council has awarded £71,740 to investigate the effects of these salts. The work will be carried out in the Department of Biochemistry and at High Royds Psychiatric Hospital, near Leeds. So far tests have shown that lithium therapy appears to reduce the frequency of manic and depressive episodes or attacks experienced by “manic depressive” patients. This is a large group of people whose otherwise normal lives are interrupted at intervals by either manic or depressive phases which put them back into hospital.
If further research confirms that lithium therapy is effective, then it’s use could become widespread. Research workers from the Departments of Psychiatry and Biochemistry, together with technical staff of the 20 bed Metabolic Research Unit at the 2,000 – bed High Royds Hospital, will carry out many more tests before any firm conclusions can be drawn. The unit is equipped to monitor the diet and bodily reaction of each patient in great detail. The tests may last for several weeks and careful control is necessary because of the number of possible variables. Quite apart from the effects of lithium, the patient might get better spontaneously or the patient might, when in hospital, be relieved of the stressful situation he has to face when at home or at work and might recover without treatment. Out-patients are also being treated with lithium salts to counteract the environmental factors in the tests. Professor Max Hamilton of the Department of Psychiatry has designed programmes so that test results can be analysed by the University main computer. Results after 3 year trials show, for example, that of 36 patients who have been treated for more than 2 years, 23 had no relapses. Previously these patients had an annual average of at least one depressive and/or manic episode over the previous 5 years. The Medical Research Council grant will enable the research unit to double its scientific staff, step up it’s investigations into the effects of lithium and also to investigate the psychiatric effects of other inorganic and organic substances.
The Metabolic Research Unit at High Royds is one of just four in the United Kingdom and was started eight years ago on the initiative of the holder of the new grant, Dr. R. P. Hullin, and Dr. R. McDonald, Medical
……………………………………………………………………………………
From Ronald Faux
Leeds, Feb 4. 1970
A £70,000 Medical Research Council Grant has been awarded to help research by Leeds University into the use of Lithium Salts as a preventive for patients liable to attacks of depression.
Results so far have been encouraging. Of 36 patients treated for more than two years, 24 have had no relapses. They had averaged at least one depressive or manic depressive attack each year over the previous five years.
If it is proved that lithium salts can be used as a prophylactic it will be an important step in the treatment of recurrent depression, which now relies entirely on drugs administered after an attack.
The treatment might also prove effective for recurrent manias ( periods of excessive mental excitement).
Dr. R. P . Hullin, senior lecturer in Biochemistry at Leeds University, will head the research with Dr. R. McDonald, medical director at High Royds psychiatric hospital, near Leeds.
The research could be important both for patients whose lives are continually disrupted by attacks of depression and for the hospitals who must provide beds for them, Dr. Hullin said. Recurrent depression accounted for about 30 per cent of all mental illness.
…………………………………………………………………………………..
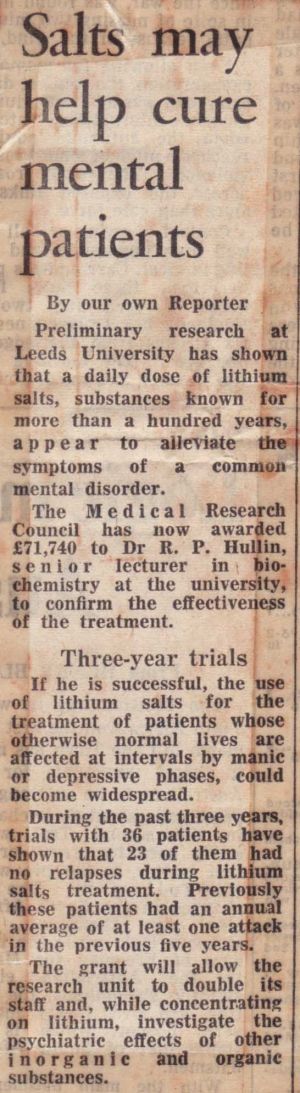
Salts may help cure mental patients
The Guardian 1970.
Preliminary research at Leeds University has shown that a daily dose of lithium salts, substances known for more than a hundred years appear to alleviate the symptoms of a common mental disorder.
The Medical Research Council has now awarded £71,740 to Dr.R.P.Hullin, senior lecturer in biochemistry at the university to confirm the effectiveness of the treatment.
If he is successful, the use of lithium salts for the treatment of patients whose otherwise normal lives are affected at intervals by manic or depressive phases, could become widespread.
During the past three years, trials with 36 patients have shown that 23 of them have had no relapses during lithium salts treatment. Previously these patients had an annual average of at least one attack in the previous five years.
The grant will allow the research unit to double it’s staff and, while concentrating on lithium, investigate the psychiatric effects of other inorganic and organic substances.
………………………………………………………………………………………
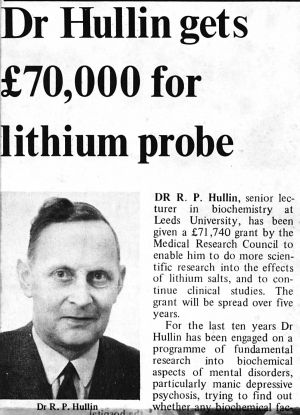
Dr Hullin gets £70,000 for lithium probe.
Dr. R. P. Hullin, senior lecturer in biochemistry at Leeds University, has been given a  £71,740 grant by the Medical Research Council to enable him to do more scientific research into the effects of lithium salts, and to continue clinical studies. The grant will be spread over five years.
For the last ten years Dr Hullin has been engaged on a programme of fundamental research into biochemical aspects of mental disorders, particularly manic depressive psychosis, trying to find out whether any biochemical factors were associated with the disease itself. He established that certain biochemical changes with respect to water content and sodium content of the cells, did change in a certain direction.
“It was in an effort to see whether modifying or reversing these biochemical changes would have any effects on the mental changes that in 1964 we began looking at lithium salts” he says. “In Denmark these had been used as an anti manic agent for a number of years.” They were not used in the Anglo Saxon world largely because there had been lithium fatalities in 1948 when these materials had been used for psychiatric reasons, but as a salt substitute in people who had been put on a low salt diet.
“It now appears that it was just unfortunate. I am not saying that they are not potentially toxic material but in this original fatality report these patients had been cardio-vascular or renal risks put on a low salt diet and under these circumstances lithium goes into the cells more rapidly.
“We began using them as anti-manic agents largely to see if they affected biochemical changes and were able to confirm that psychiatrically they did have an anti-manic effect in a high proportion of manic patients and that they did have some modifying influence on changes we had previously demonstrated.
“Around that time another report came from Denmark claiming that these salts in somewhat lower doses also had a preventive effect against not only mania but this manic depressive condition including recurrent depression. If true this could result in wide clinical use of this drug. It is this side that we have been investigating both biochemically and psychiatrically.”
The drug has been tested on 75 patients who before being put on lithium had at least one episode of depression or mania per year for the preceding five years. Thirty six had been on lithium for periods of two to three years and twenty four of them have had no relapses at all.
“If we are able to determine the location of biochemical or metabolic effects of lithium within the body, it would give us a clue to the actual disease itself,” says Dr. Hullin.
…………………………………………………………………………………..
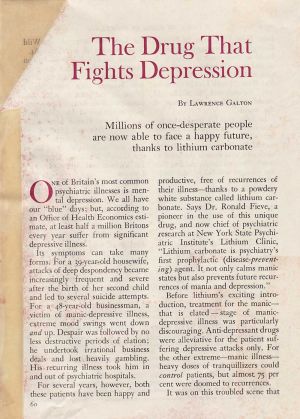
May 1976, Readers Digest.
The Drug That Fights Depression
By Lawrence Galton
Millions of once-desperate people are now able to face a happy future thanks to lithium carbonate.
One of Britain’s most common psychiatric illnesses is mental depression. We all have our depressing days; but according to an Office of Health Economics estimate, at least half a million Britons every year suffer from significant depressive illness.
Its symptoms can take many forms. For a 39 year old housewife, attacks of despondency became increasingly frequent and severe after the birth of her second child and led to several suicide attempts. For a 48 year old businessman, a victim of manic-depressive illness, extreme mood swings went down and up. Despair was followed by no less destructive periods of elation; he undertook irrational business deals and lost heavily gambling. His recurring illness took him in and out of psychiatric hospitals.
For several years, however, both of these patients have been happy and productive, free of recurrences of their illness thanks to a powdery white substance called lithium carbonate. Says Dr. Ronald Fieve, a pioneer in the use of this unique drug and now chief of psychiatric research at New York State Psychiatric Institutes Lithium Clinic, Lithium carbonate is psychiatry’s first prophylactic (disease preventing) agent. It not only calms manic states but also prevents future recurrences of mania and depression. Before lithium’s exciting introduction, treatment for the manic, that is the elated stage of manic depressive illness was particularly discouraging. Anti depressant drugs were alleviative for the patient suffering depressive attacks only. For the other extreme manic illness heavy tranquillisers could control patients, but almost 75 per cent were doomed to recurrences. It was on this troubled scene that lithium made its entrance. Lithium, in the form of its chloride salt, had been used in the 1940s as a popular salt substitute for people on sodium free diets. Then came tragedy. Several deaths and serious poisonings were attributed to lithium chloride. Lithium, it was realised, could be dangerous for patients with congestive heart and kidney diseases.
In 1949, however, Dr. John Cade, an Australian psychiatrist, was discovering the value of lithium against mania. Cade found that manic depressive illness might be the result of a fault in body chemistry, much like diabetes and hypothyroidism. He injected urine from manic patients into guinea pigs and observed a toxic effect. When he tried injecting lithium carbonate into the guinea pigs, he found that it exerted a marked calming effect.
Cade then gave lithium carbonate to ten patients during the manic phase of their illness. In every case within two weeks the mania disappeared. Two years later, similar results in 30 other patients were reported by other Australian psychiatrists, who also noted that when lithium was continued on a maintenance dosage it appeared to prevent recurrent attacks. But the idea of prophylaxis for a mental illness was so startling that it was debated for years, Still, confirmation began to come through. British psychiatrist Geoffrey Hartiga in a small hospital study, found that six out of eight depressive patients treated with lithium remained symptom-free for three years or more. Two Danish Investigators, Mogens Schou and Poul Baastrup, were achieving encouraging results on a far wider scale. In one study, 88 women who had suffered manic-depressive episodes received lithium and were observed for 78months. Previously the women had experienced episodes on an average of every eight months. On lithium, many went for five years and more without a relapse.
More follow up research in Britain produced equally satisfactory results. Dr. Alec Coppen, director of the Medical Research Councillors Neuropsychiatry Unit at West Park Hospital in Surrey, headed a two year survey of 65 depressive and manic-depressive patients in four hospitals. Of 28 patients on lithium, 24 showed little or no disorders, compared with only three of the 37 patients in a control group receiving placebo (identical-looking but inert)tablets. Also, patients not receiving active lithium needed far more conventional treatment; and 43 per cent received electro convulsive therapy, compared with none in the lithium group.
Dr.Roy Hullin, Dr. Robert McDonald and Dr. Michael Allsopp tried lithium treatment over an average period of 50 months on 95 patients attending High Royds Hospital at Menston in Yorkshire. Time spent in hospital went down from an average of nearly 30 weeks a patient to four weeks. Two thirds of the patients were not in hospital at all while receiving lithium. Says Dr.Hullin : Our trials have convinced us that, with careful monitoring, most manic-depressives can be treated entirely as outpatients.
Lithium carbonate has also been found valuable for patients who suffer recurrent depression symptoms only. American studies in 18 hospitals over a four year period concluded that lithium with regular clinical appraisals appears to be a safe and effective treatment for preventing such episodes.
A new Medical Research Council multi-centre trial of lithium as a preventive against depression has just started in Leeds, Edinburgh, Sheffield, Southampton, Dundee and Cardiff. Some 200 patients will be involved; results may eventually benefit many of the 80,000 Britons suffering from recurrent depression.
In excessive doses, lithium can be poisonous ( as virtually any useful drug can be) and some patients experience unpleasant side effects. But there are now clear guidelines for lithium’s safe use. At High Royds Hospital Lithium Clinic, for instance, where 300 people are currently being treated, new patients are seen by a doctor once a week until they are stabilised on lithium and are clinically well. Thereafter they come to the clinic once every four weeks for evaluation, behaviour and mood ratings, and for the taking of blood samples to test blood lithium levels and thyroid function. After six months, attendance is normally reduced to once every eight to 12 weeks.
If you suspect that you or someone close to you has a depressive problem, tell your family doctor about it. Depression should be considered a possibility whenever social, sexual or vocational life is markedly disturbed by a mood swing. Especially if the swing is cyclical with highs and lows or repeated lows the problem may not be psychological but, rather, chemical, and may possibly be alleviated by the use of lithium therapy.
A patient suffering from a depressive disorder will probably be referred by his GP to a consultant psychiatrist at his local hospital. If lithium is prescribed, there is every likelihood he will be able to receive treatment as an outpatient, either in the hospitals psychiatry department or at a special lithium clinic if there is one near by. And after the initial tests and medication, treatment will be straightforward; he will simply have to take a daily dose of lithium tablets at home, and attend the hospital or clinic for regular check ups.
ROBERT MCDONALD, formerly Consultant
Psychiatrist and Medical Director, High Royds
Hospital, Menston,Nr Ilkley
Bob McDonald died at his home in Ilkley on 7 October 1990 at the age of 75, after a long period of illness. He was born on 4 May 1915 in Aberdeen, where he later graduated MB, ChB in 1937and after junior hospital appointments he eventually entered general practice in Manchester until 1946. He then returned to Aberdeen and took the DPH, followed by appointment as a registrar at High Royds Hospital, Menston, obtaining his DPM in 1949. After more senior posts at Hellingley Hospital and St James’s, Portsmouth, he was appointed consultant psychiatrist at St George’s, Morpeth in 1953: he took up his final appointment at High Royds Hospital some seven years later, retiring in 1979.
His time at High Royds was one of great change and considerable difficulty, with conflicting philosophies of care and corresponding conflicts among some of his colleagues. As medical director, it fell to his lot to plan and facilitate the changes necessary to transform a large institution with many long-stay patients to a more modern and dynamic hospital, and yet to pave the way for its eventual closure. Throughout, his clear sense of purpose, determination and his deep and genuine concern for the patients-especially the long-stay-enabled the necessary changes to occur without too much upheaval. In addition he played an active part in the setting-up and the clinical work of a metabolic research unit within the hospital for the study of recurrent affective disorders and their treatment by lithium salts, in which he was influenced by the work of Mogens Schou in Denmark, whom he knew well.
He became a Senior Clinical Lecturer in the Leeds University Department of Psychiatry, a Mental Health Tribunal professional member and a member of the Home Office Panel of Psychiatrists for prison referrals, and was elected FRCPsych. in 1971.
An essentially very private man, Robert McDonald did not court popularity but always gave of his best, particularly where the welfare of his patients was involved, and they could always rely on his help and understanding. His last few years were marked by illness and major surgery and though often in pain, he bore it with the stoical fortitude which always characterised his reaction to the vicissitudes of life.
He is survived by his Danish wife, Helen, a son and daughter and four grandchildren.
JMR
………………………………………………………………………………………………………
Mental care put top priority
Yorkshire Post Reporter.
Improvement of mental health facilities should be the main target, members of Yorkshire Regional Health Authority decided yesterday after discussing long term strategic objectives.
The objectives, in a consultation document which district health authorities will discuss, should be finalised and included in a regional strategic plan by March, 1985.
Other priority aims, in no particular order recommended are: provision of adequate services for the elderly; rationalisation of acute sector services; relocation of isolated maternity units, development of community and home care services and of facilities for the younger physically disabled.
The document follows national and regional guidelines and priorities could be adjusted following comment by districts.
Dr.Julian Roberts, a psychiatrist, said that the bulk of services for the mentally handicapped throughout the region were centred in large old institutions.
“I think our priority should be in the field of mental illness and handicap. In the mental handicap field, progress will be more difficult because it involves local authorities,” said Dr. Roberts.
“We can’t expect to put people back into the community in local authority care without adequate funding. If we did we would be failing on our duty to patients,” he added.
Dr. Roy Hullin, vice-chairman said it was important to recognise that during the period for which they were planning (1985-1995), the number of people over 75 with greatly increased health care needs in the region would rise by 11 per cent.
“It is crucial that the thrust towards community care for the mentally handicapped, the long term mentally ill and the elderly must not be made an excuse for people falling between two stools.
“Community care, properly carried out, is not a cheap alternative to hospital care and there is a danger that people will be discharged from hospital in the belief that proper community care will be provided.
“It could be dangerous if this thrust towards community care was not accompanied by proper facilities within the community. That would be the Health Service getting rid of some of its problems in the mistaken hope that other people would pick up the tabs,” added Dr.Hullin.
Coun.Eric Pickles, of Bradford (Con, Worth Valley), said it seemed that while everyone was prepared to pay lip service to community care, nobody was prepared to back it up with adequate resources.
It was decided to set up a working party to look into the financial implications of transferring more patients from institutional to community care.
Members supported a Wakefield Health Authority proposal to close a 24 bed ward for chest patients at Snapethorpe Hospital. This will result in the hospital’s temporary closure until it’s long term future is decided and patients being referred to Pinderfield’s Hospital.
Because of objections by the Community Health Council, the Secretary of State will make a final decision on the ward closure.